Buprenorphine is an established treatment for opioid disorder ¹
About Buprenorphine
Buprenorphine (BPN) is an established treatment for opioid use disorder¹.
Buprenorphine is most commonly given as a daily tablet that dissolves under the tongue or on the inside of the mouth².
Buvidal is the first long-acting, injectable form of buprenorphine available in the UK.
When used at an appropriate dose for Opioid Dependence Treatment, buprenorphine is able to simultaneously suppress withdrawal and cravings (substitute for other opioids) and to block the subjective effects of additional opioid use3,4.
How buprenorphine works1,4,5
Buprenorphine acts as a partial agonist at the mu-opioid receptor (MOR).
It has high receptor affinity, meaning it binds tightly to the mu-receptor and has low intrinsic activity, meaning it stimulates a relatively low receptor response, compared with full agonists, such as heroin or methadone.
Conceptually, this means that buprenorphine is more strongly attracted to the opioid receptors in the brain than heroin (and methadone) and binds very tightly to them. It binds so tightly to the receptors, that, if dosed optimally, taking other opioids has little or no subjective effect. This is because it is difficult (although not impossible) for other opioids to displace buprenorphine from receptors. It is important to note that, at a high enough relative dose, heroin or another opioids could out-compete buprenorphine and overcome this blockade effect.
In someone who is opioid dependent, signs and symptoms of opioid withdrawal are suppressed when a certain level of mu-opioid receptor activation is maintained. If buprenorphine is given to someone who still has a full opioid agonist like heroin or methadone in their system, they may go into immediate (‘precipitated’) withdrawal. This is because the buprenorphine can block the effect of the full agonist, without fully replacing it. Precipitated withdrawal may discourage people from continuing with treatment.
The risk of precipitated withdrawal can be minimised by waiting until mild-to moderate opioid withdrawal is present before giving the first dose of buprenorphine. When planning a buprenorphine initiation, it is important to take into consideration whether the person is taking a long or a short acting opioid to ensure sufficient time between discontinuation and the first dose of buprenorphine.
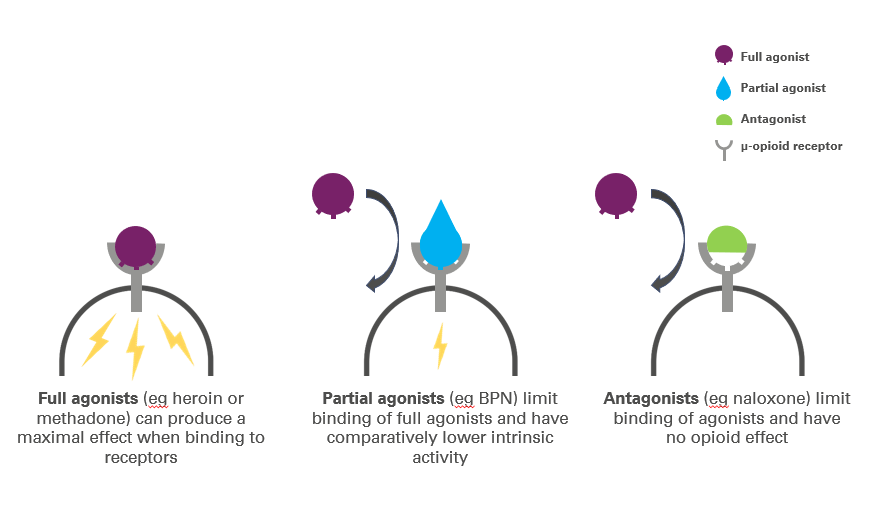
We’ve created a short video to explain how different types of drugs interact with opioid receptors within the body and how buprenorphine specifically can suppress withdrawal and cravings and block the subjective effects of additional opioid use1,3,5
Buprenorphine within a treatment framework
If choosing buprenorphine as a treatment option, it is important that there is a comprehensive care plan that addresses the range of social and psychological challenges that each individual faces⁶.
Buprenorphine and respiratory depression5,7
Buprenorphine has a relative “ceiling effect” on respiratory depression. This may result in a lower risk of overdose with buprenorphine compared with a full agonist such as methadone. The comparative effect on respiratory depression between Buvidal and other opioid medications has not been evaluated.
Buprenorphine can cause serious respiratory depression, especially when it is used in combination with other central nervous system depressant drugs such as benzodiazepines, gabapentinoids, or alcohol.
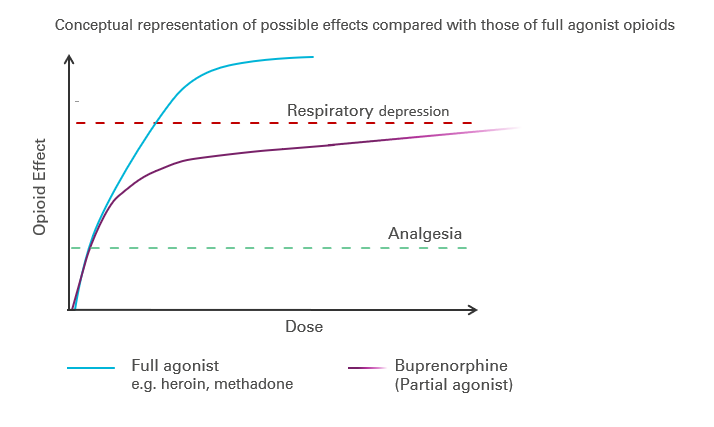
* Graphical representation adapted from reference 5